Texas A&M Professors Collaborate to Take Up Fight Against Emerging Zoonotic Disease
A disease most people have never heard of, which has come to the Americas only in the last year, may soon become a major public health issue in the United States. Chikungunya (pronunciation: chik-en-gun-ye) virus has been recognized as the cause of periodic epidemics in Africa and Asia since the 1950s and has now spread to all but six countries in the Americas, with over 1.4 million suspected cases since first arriving in the Caribbean in late 2013. There have been 11 cases thus far reported in Florida where the patient had not reported any recent travel.
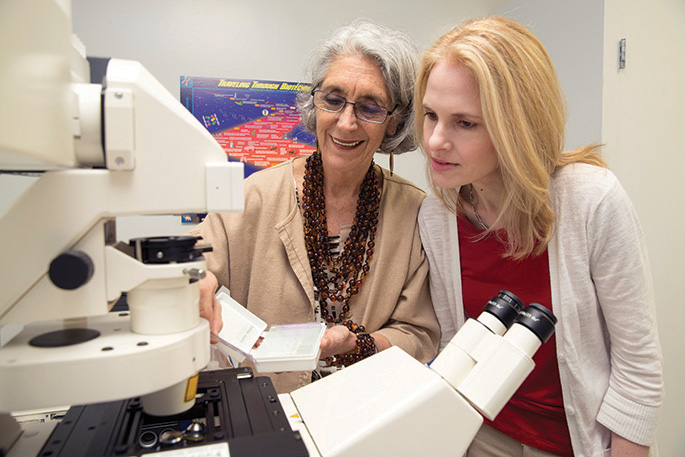
“We have local transmission in the United States,” said Dr. Rosina “Tammi” Krecek, a visiting professor and interim assistant dean of One Health at the Texas A&M College of Veterinary Medicine & Biomedical Sciences (CVM). “We also have imported transmission. An example of local transmission is ‘I didn’t leave home, a mosquito bit me, and I became infected.’ Imported transmission is ‘I flew to an endemic country, a mosquito bit me, and I became infected and returned with the infection.'”
The chikungunya virus is spread among humans by the bite of either of two species of mosquitoes: Aedes aegypti (“yellow fever mosquito”) and, less commonly, Aedes albopictus (“tiger mosquito”). When the mosquito bites an infected person and then subsequently bites a healthy individual, the virus can be transferred to that second person. Aedes aegypti can be found in the southeastern United States from Texas to South Carolina, while Aedes albopictus can be found as far north as New York City.
“In some parts of the country, there’s really no risk of initiating transmission, but anywhere in the southeast, there is a risk, especially during the summer,” said Dr. Scott C. Weaver, director of the Institute for Human Infections and Immunity at The University of Texas Medical Branch at Galveston, who collaborates with Krecek and others at Texas A&M on this disease.
One worry the scientists have is that if the virus were to mutate to make it more easily spread by Aedes albopictus mosquitoes, a much larger percentage of the United States population could be affected.
Health officials in the Caribbean are urging businesses and individuals to eliminate standing water and take other precautionary measures against mosquitoes. Unfortunately, these kinds of mosquitoes tend to thrive in urban areas, including inside buildings, so simply fumigating the outside areas with insecticide is unlikely to have much effect. Therefore, travelers must take it upon themselves to exercise reasonable precautions, including wearing mosquito repellent and sleeping in rooms with screened windows, air conditioning, or mosquito netting. As there is no treatment or vaccine for the chikungunya virus, preventing mosquito bites remains the only defense.
Chikungunya virus comprises a clear example of One Health defined as the inextricable link between animal, human, and environmental health. Because animals and the environment are considered important factors in human disease, the best way to combat a virus like chikungunya is a One Health approach. Furthermore, humans are not the only ones who can become infected. “There is some evidence that animals-including non-human primates, small mammals, and birds-may act as reservoirs for the virus,” said Dr. Christine Budke, an associate professor at the CVM. “However, because it’s a new virus to this part of the world, there’s very little information on non-human reservoirs in the Americas.”
“There is a risk that the virus could use non-human reservoirs in South and Central America, where there are plenty of wild primates, but we simply don’t know if those species are competent to serve as reservoir hosts,” Weaver said. “We also don’t know if the mosquitoes that are present in the forest habitats where those monkeys live would be competent to transmit in a monkey/mosquito cycle, like exists in Africa.”
Other factors affecting the transmission of the virus may include movement of people and animals as well as changes in climate, but how that works is also largely unknown. “We don’t fully understand the role of the mosquito or the role of climate in the disease cycle,” Krecek said. “We don’t know how the mosquito is influenced by the environment. For example, what leads to a more, or less hospitable habitat for the vector?”
As of January 1, 2015, chikungunya is a reportable disease, meaning doctors must tell the Centers for Disease Control and Prevention (CDC) of any cases. Although this move demonstrates the CDC’s concern about this virus, experts say it is unlikely to result in increased numbers of cases reported, as doctors already generally report any cases they see of this unusual virus.
An issue is that this disease mimics other, more common diseases. Symptoms typically begin, three to seven days after being bitten by an infected mosquito, with a sudden high fever and joint pain, often followed by headaches, muscle pain, coughing, joint swelling, and/or a rash. Although the disease is rarely life threatening and symptoms subside in many people within a few weeks, for some of those with the disease (estimated at up to 60 percent by some studies), the joint pain may last for months or even years and can be so debilitating they are unable to go about their normal lives.
“I’ve received emails from a lot of people here in the United States who have become infected, travelers mostly,” Weaver said. “They’re a month or two out after their infection, and they’re still experiencing severe arthralgia and asking about experimental treatments, or anything else that they can do. Unfortunately, there’s not much other than our typical non-steroidal anti-inflammatory drugs that you would take for pain and swelling for people with chikungunya.”


