Discovering A Passion For Equine Medicine
Alex Pastis, a fourth-year Texas A&M Doctor of Veterinary Medicine (DVM) student and future equine veterinarian, proves that passion is a strong, almost unstoppable force. While, unlike many of his peers, Pastis didn’t consider becoming a veterinarian until his freshman year in college, once he’d gained an affinity for the field, his pursuit of a […]
Australian Timor Ponies Have Genetic Diversity Necessary For Breeding Program, Texas A&M Researchers Find
The tropical breed may prove vital to Australia as global warming continues to cause climate changes. Researchers at the Texas A&M School of Veterinary Medicine & Biomedical Sciences (VMBS) collaborated with Australian geneticists to determine whether the country’s population of Timor ponies are genetically diverse enough to support a designated breeding program. Timor ponies, which […]
Texas A&M Veterinarians Leave No Stone Unturned In Diagnosing Horse’s Mysterious Colic
When Koche, an American Paint Horse, began experiencing recurring bouts of colic, her owner, Cedrick Harvey, was determined to discover the source of the problem because of the 7-year-old mare’s special place in his family. “Her grandmother was an amazing Paint horse named Apache that grew up within our family,” Harvey said. “We really wanted […]
Next Steps For Controlling Equine Colitis
Among the numerous gastrointestinal disorders affecting horses, colitis can be a challenging and potentially serious condition, depending on the severity of the horse’s symptoms and the condition’s underlying cause. Dr. Amanda Trimble, a clinical assistant professor of equine internal medicine at the Texas A&M School of Veterinary Medicine & Biomedical Sciences, explores how owners can […]
Staying On Guard Against Equine Colitis
Horses have delicate and complex gastrointestinal systems compared to many other animals, leaving them susceptible to digestive disorders, such as colitis. “The term ‘colitis’ means inflammation of the large intestine, which is most often accompanied by diarrhea,” explained Dr. Amanda Trimble, a clinical assistant professor of equine internal medicine at the Texas A&M School of Veterinary Medicine […]
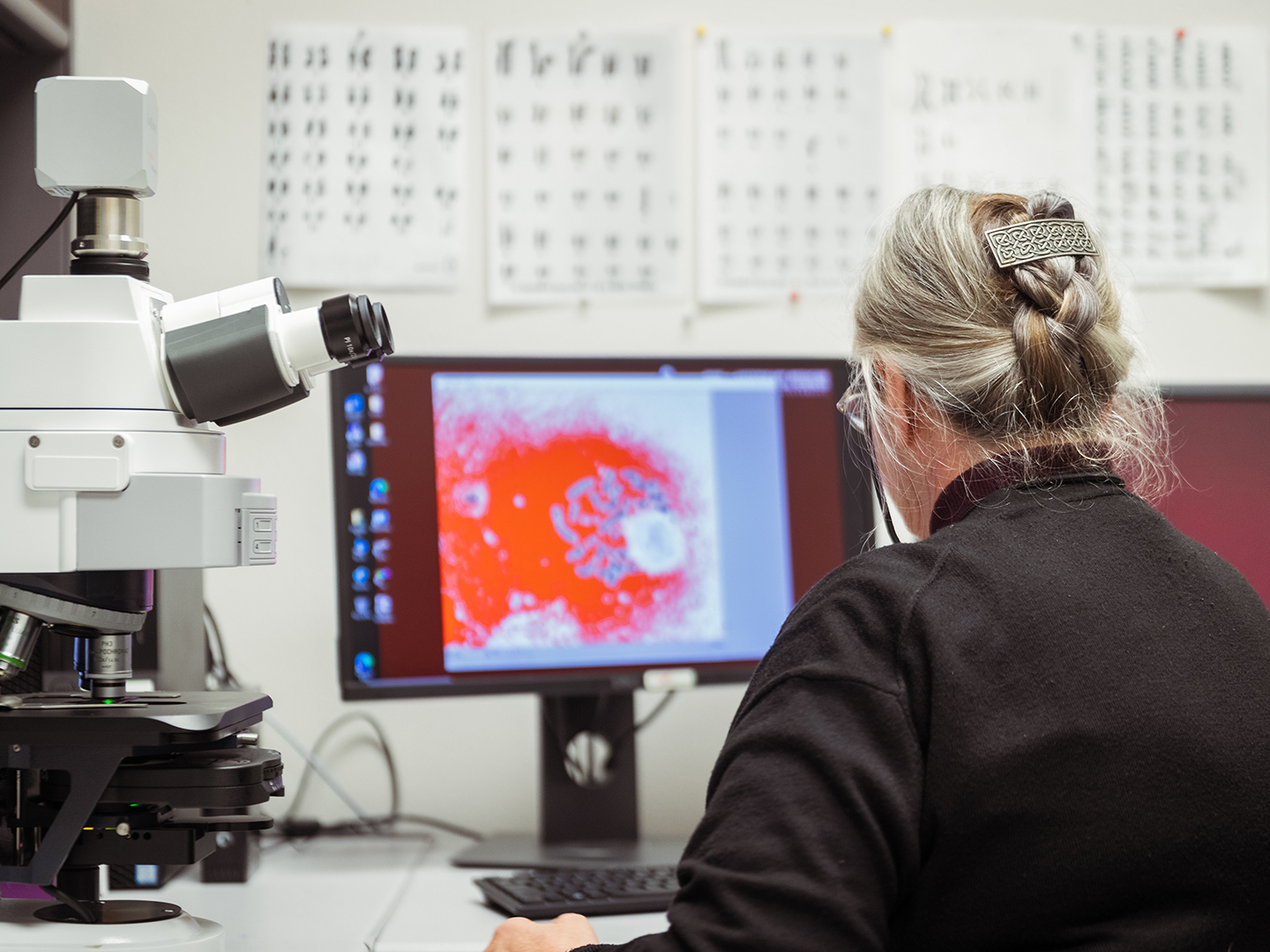
Texas A&M Researchers Studying Reproductive Abnormalities That Cause Sterility In Horses
Researchers at the Texas A&M School of Veterinary Medicine & Biomedical Sciences (VMBS) have received a $640,000 grant from the United States Department of Agriculture (USDA) to study abnormalities in sex development that affect the reproductive capabilities of some horses. The new project will examine a diverse group of about 100 sterile horses, including those […]
Good Karma: Aggie Veterinarians Save Horse From Life-Threatening Melanoma
Teresa Porter has been taking care of horses for decades, but none have touched her heart like Karma. Karma, known at competitions as So Riveting, is a 20-year-old quarter horse stallion with a striking gray coat. But with that color comes a problem — gray horses are genetically predisposed to developing melanoma, especially on body […]
Navigating The Mysteries of Gray Horse Melanoma
Horse ownership offers many joys, but as owners navigate the needs of their equine companions, they may find that each breed has its own unique requirements. What owners may not know is specific coat colors can signal distinct health challenges that they should attentively watch for and address. In the spirit of National Day of […]
Texas A&M Veterinarians Help Horse Recover From Life-Threatening Botulism
Thanks to the quick thinking of veterinarians from the Texas A&M Large Animal Teaching Hospital (LATH), a horse named Tesoro is back on his feet after a frightening case of botulism, a disease not common in Texas. Sydney Reed, a pre-veterinary animal science student at Texas A&M University, purchased Tesoro, a quarter horse gelding, as […]
Helping Horses With Equine Asthma Breathe Easier
Although asthma symptoms generally worsen in the winter for horses because of the cold, dry air, summer weather can also “stirrup” trouble for horses with a specific form of asthma — summer pasture associated asthma. “Equine asthma — also known as inflammatory airway disease (IAD), recurrent airway obstruction (RAO), or ‘heaves’ — is a common […]