Father’s Alcohol Consumption Before Conception Linked To Brain And Facial Defects In Offspring
Fetal alcohol syndrome-related craniofacial differences could be seen in offspring born to fathers who regularly consumed alcohol to the legal limit. According to the U.S. Surgeon General, women should not drink alcoholic beverages during pregnancy because of the risk of birth defects in their unborn child. However, research at Texas A&M University now demonstrates that […]
Texas A&M Researchers Detail Groundbreaking Angelman Syndrome Development
A new publication explains the novel science behind the first molecular therapeutic for the rare neurogenetic disorder to advance into clinical development. Researchers at Texas A&M University have developed the first molecular therapeutic for Angelman syndrome to advance into clinical development. In a new article, published today in Science Translational Medicine, Dr. Scott Dindot, an […]
Texas A&M Researchers Play Key Role In National Animal COVID-19 Research
Nine Texas A&M University researchers made key contributions to the first national-scale COVID-19 animal surveillance study that analyzed companion animal COVID-19 data from across the United States. The study was led by the Centers for Disease Control and Prevention (CDC) and aimed to characterize the clinical and epidemiological features of COVID-19 in companion animals. The […]
Texas A&M, Carnegie Mellon Researchers Test Air Pollution In East Palestine, Confirm EPA’s Findings But Identify Future Needs For Continued Sampling
Additional data was released by the Texas A&M Superfund Center on March 9 and is available on Twitter. Independent data collection by the Texas A&M Superfund Research Center and Carnegie Mellon University has corroborated the U.S. Environmental Protection Agency’s (EPA) findings on air quality in East Palestine, Ohio. Researchers from the two universities, both partners in […]
Texas A&M University Spotlights Immunology Research At Inaugural Symposium
Four units at Texas A&M University recently came together to host a symposium highlighting research projects occurring across the state and beyond in the vast field of immunology. The inaugural Texas Symposium on Critical Topics in Immunology took place on Feb. 17-18 and was co-sponsored by the university’s Hagler Institute for Advanced Study, School of […]
Exercise Has A Direct Role In Fighting Breast Cancer, Finds Texas A&M Study
While it is generally accepted that exercise can benefit a person’s overall health, a recently published paper has found a direct link between muscle contraction and a reduction in breast cancer. In the paper, published in the journal Frontiers in Physiology, a team of Texas A&M researchers concludes that a currently unspecified factor released during […]
VMBS, VERO Make Impact At Animal Disease Research Conference
Thirty-three student and faculty researchers from the Texas A&M School of Veterinary Medicine and Biomedical Sciences (VMBS) made a splash with their research presentations at the 103rd Conference of Research Workers in Animal Diseases (CRWAD). The VMBS representatives presented research to an audience of more than 600 scientists from around the world at CRWAD 2023, […]
Texas A&M Postdoc Receives NIH Grant For Toxicology Research
Dr. Meichen Wang, a postdoctoral trainee in Texas A&M University’s Interdisciplinary Faculty of Toxicology, has been awarded a nearly $1 million career development grant from the National Institute of Environmental Health Sciences, one of the National Institutes of Health (NIH). Wang’s grant, an NIH Pathway to Independence Award (K99/R00), will provide support for her work […]
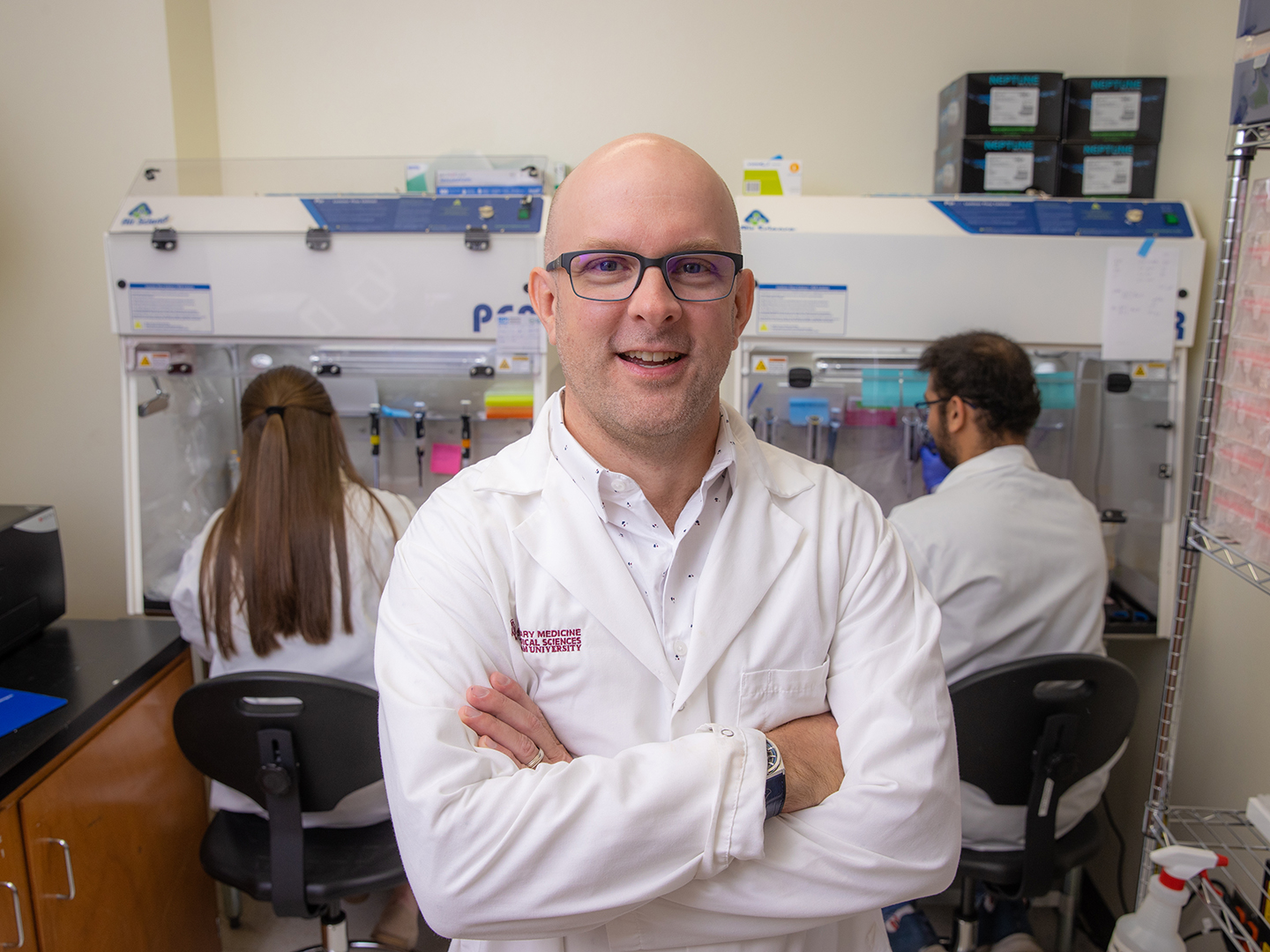
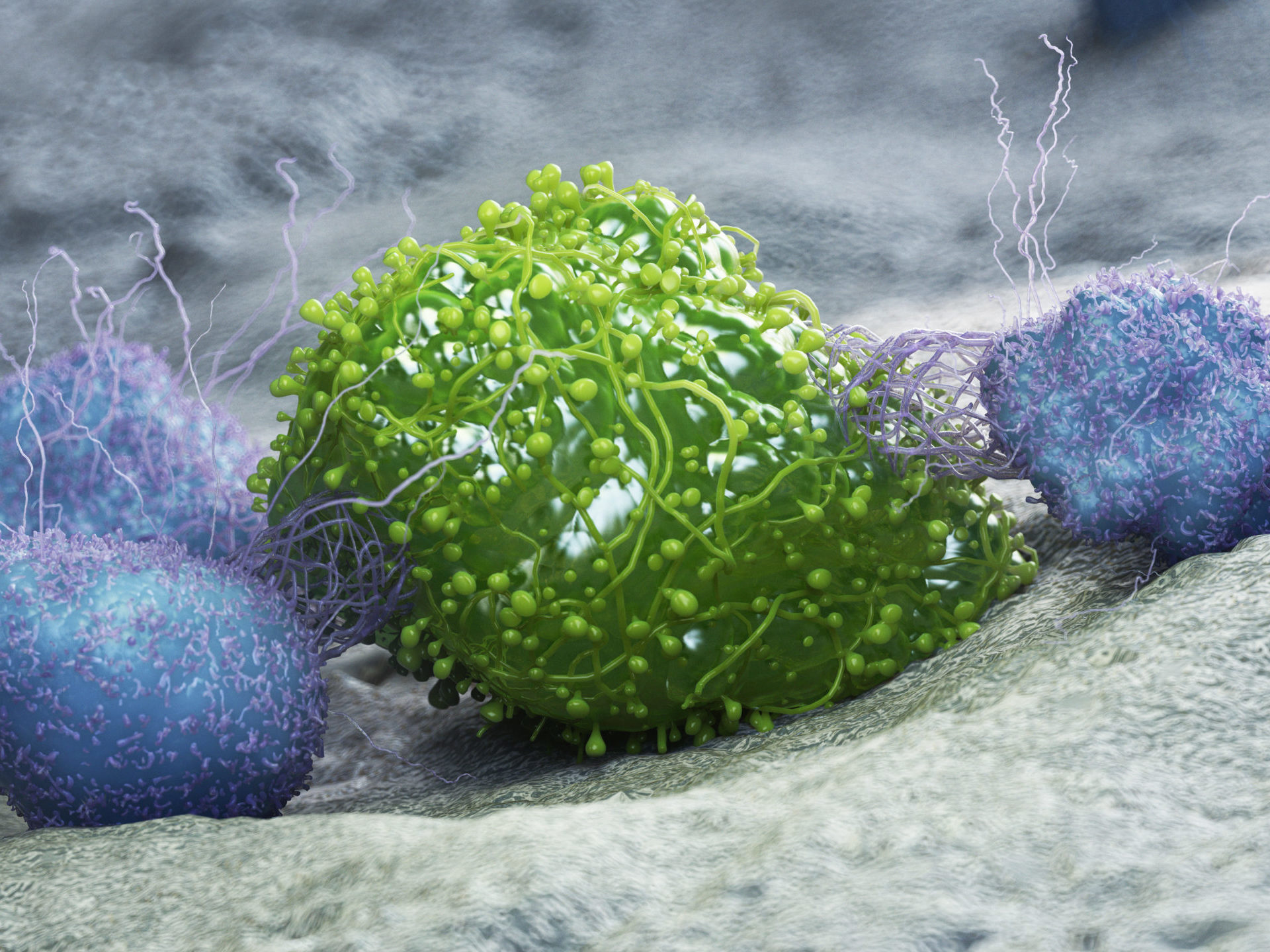
Texas A&M Researchers To Further Develop Unique Cancer Drug With $2.3M NIH Grant
Preliminary data indicate that the compounds developed in the laboratory of Dr. Stephen Safe both kill tumors and rejuvenate the immune system, which becomes exhausted as it responds to cancer. A team of Texas A&M University researchers has received a $2.3-millon grant from the National Institutes of Health to further explore a unique immunotherapy that […]
Texas A&M Is Home To World’s Top Two Dog Experts
In addition to employing the top two experts on the topic, Texas A&M University is listed as the world’s fifth most knowledgeable institution on dogs. The top two experts on dogs in the world are faculty members at the Texas A&M School of Veterinary Medicine & Biomedical Sciences (VMBS), according to the life sciences search […]