Texas A&M, Vet Valor Fund Help Get ‘Lieutenant Dan’ Back On His Feet With Hip Surgery
Lieutenant Dan, a three-legged mixed breed dog, wears a tag that says, “Got no leg,” but his lack of a limb doesn’t slow him down. Like his namesake from “Forrest Gump,” this Lieutenant Dan faced a life-altering challenge when he lost one of his hind legs; unlike the character Lt. Dan, however, the canine Lieutenant […]
A Little Dog With A Lot Of Heart: Texas A&M Veterinarians Help Chihuahua Overcome Life-Threatening Heartworm Complication
An 8-pound Chihuahua named Petey McPherson holds a new record at the Texas A&M Small Animal Teaching Hospital (SATH) after having 58 heartworms surgically removed from his tiny heart. This overwhelming number of heartworms would have been fatal for Petey if his loving owner, Don McPherson, had not rescued him as a stray and ensured […]
Helping Hammie Breathe Easy: Texas A&M Veterinarians Save Cat With Windpipe Obstruction
Hammie, an orange tabby, had a rough beginning — he started life as a feral kitten outside a prison in Huntsville, Texas, and even after being rescued by one of the prison’s nurses, his challenges weren’t over. After Hammie developed an unusual cough, his veterinarian detected a foreign object in his windpipe that was obstructing […]
Texas A&M Oncology Team Helps Top Police K-9 Overcome Cancer
Texas DPS handler makes weekly two-hour trips for K-9 partner’s cancer treatment. Police K-9 Athena and her handler Josh Perkins have been an unstoppable pair in their service to the Texas Department of Public Safety (DPS); since they began working together, the two have broken several records across the state and received multiple awards. While […]
From Feral To Fur-ever: Texas A&M Gives Cat Third Chance After Mammary Cancer Diagnosis
A chance encounter at a Houston loading dock in 2016 set the stage for an incredible journey of survival and transformation for Alice, a feral mother cat. When Tobi Kosanke, a geologist from the Houston area, originally brought Alice home, the kitty was so scared of people that she hid from her rescuers for half […]
Texas A&M Equine Theriogenology Service Extends A Beloved Donkey’s Legacy
As any animal lover will tell you, there’s nothing quite like the human-animal bond. For Martha and Tommy Soyars, their special connection was with Moses, a mammoth jack donkey who joined their family in 2007 as a young colt. When the couple learned that Moses was approaching the end of his life, they began to […]
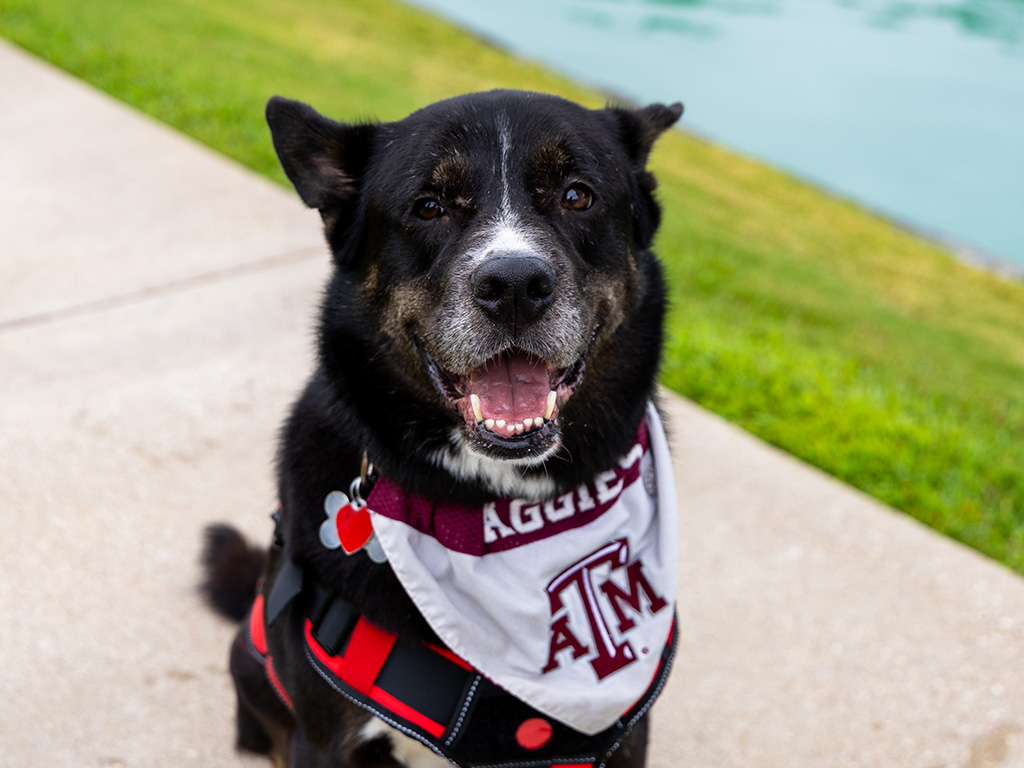
Texas A&M Veterinarians Help Service Dog Overcome Heartworms
With the help of Texas A&M experts, one family championed their beloved service dog, saving him from heartworms as repayment for the love he had given them in their times of need. When Texas A&M University freshman Paola Assanmal felt like she was at rock bottom, she found a friend in Rocky, a 4-year-old pit […]
Texas A&M Veterinarians Help Donkey Foal Fight Critical Health Issues
If there is one word that Stefanie Shaver, would use to describe her jenny foal, Shadow, it would be a “fighter.” “Shadow began her life struggling with several medical conditions,” Shaver said. “She’s pulled through a lot, so for her to be around today is really a godsend.” At just 2 months old, Shadow was […]
Texas A&M Veterinary Specialists Help Pug Overcome Multiple Health Conditions
Unlike her high-energy, attention-seeking siblings Canela and Choclo, Chispa the pug is lovingly described by her owner Peter Schulte as more of a “potato kind of dog.” “She just lies around,” said Schulte, who lives in downtown Houston with his partner Ramiro Flores and their three pugs. “She likes lying outside in the sun or, […]
Something To Smile About: Texas A&M Veterinarians Heal Camel With Dental Abscess
As a camel, Karl Humphrey spends his days living a blissful life with his brother Johnny at Blessington Farms, a family-friendly farm experience west of Houston. The dromedaries, or single-humped camels, help educate elementary children, families, and farm visitors about camels and the care they require. Perhaps Karl’s favorite part of the job is providing […]