Texas A&M Small Animal Teaching Hospital Welcomes New Dentist
As the Texas A&M Small Animal Teaching Hospital’s (SATH) newest veterinary dentist, Dr. Adriana Regalado is advancing veterinary dental techniques while educating Aggie veterinary students on the importance of caring for patients’ teeth. Regalado joins the SATH’s Dentistry Service as a clinical assistant professor in the Texas A&M School of Veterinary Medicine & Biomedical Sciences’ […]
Australian Shepherd Receives Three Life-Saving Surgeries At Texas A&M Veterinary Hospital
An 8-year-old Australian Shepherd named Ollie survived a monthlong onslaught of unexpected health emergencies thanks to the veterinarians, staff, and students at the Texas A&M Small Animal Teaching Hospital (SATH). During her time at the SATH, Ollie received three life-saving surgeries that began with treatment for bladder stone complications but ended with dangerous blood clots. […]
Texas A&M Veterinarians Diagnose Rare Autoimmune Disease, Put Silver Lab On Road To Recovery
Having two autoimmune diseases is unusual for a dog, but having three is exceptionally rare. When Lanie, an English silver Labrador retriever, began showing signs of another illness less than a year after the diagnosis of her first two autoimmune diseases, her owners acted quickly, taking her to their local, trusted emergency veterinary clinic. The […]
Texas A&M Veterinarians Leave No Stone Unturned In Diagnosing Horse’s Mysterious Colic
When Koche, an American Paint Horse, began experiencing recurring bouts of colic, her owner, Cedrick Harvey, was determined to discover the source of the problem because of the 7-year-old mare’s special place in his family. “Her grandmother was an amazing Paint horse named Apache that grew up within our family,” Harvey said. “We really wanted […]
Texas A&M’s New Theriogenologist Working To Solve Animal Reproductive Issues, Share Passion With Next Generation
Animal reproduction is a complicated process that requires a perfect balance of many fertility variables. Most of the time, Mother Nature knows exactly what she’s doing; after all, animals have been reproducing for millions of years without human intervention. But when certain variables — like having healthy sperm or a straightforward birth — don’t align, […]
Texas A&M Veterinary Hospital Provides Wellness Care To Animals In Underserved Areas
According to the U.S. Bureau of Labor Statistics, there were 18,810 veterinarians and veterinary technicians in Texas as of May 2022. Of those, roughly 73% are located in Texas’s largest cities, including Austin, Dallas, Houston, and San Antonio, leaving those in rural communities without easy access to veterinary care and making it harder for pets […]
Texas A&M Veterinary Clinical Trial Gives Tabby Cat With Chronic Kidney Disease A Second Chance At Life
Unlike the tender variety of Japanese beef that he’s named for, Kobe has always been one tough tabby. The now 14-year-old male has overcome numerous obstacles in life, including a rough start as a kitten and a weight loss journey from 28 pounds down to 12. “I was 8 years old when my mom found […]
Texas A&M Veterinarians Create New Strategies For Treating Ear Issues In Kangaroos
Diego the red kangaroo has an important job at the Texas A&M Winnie Carter Wildlife Center. In addition to teaching veterinary students about kangaroo care and medicine, he serves as a “seeing eye” kangaroo for his blind “roo mate,” Murdock. When Diego’s caretakers at the wildlife center noticed that he seemed to be experiencing discomfort […]
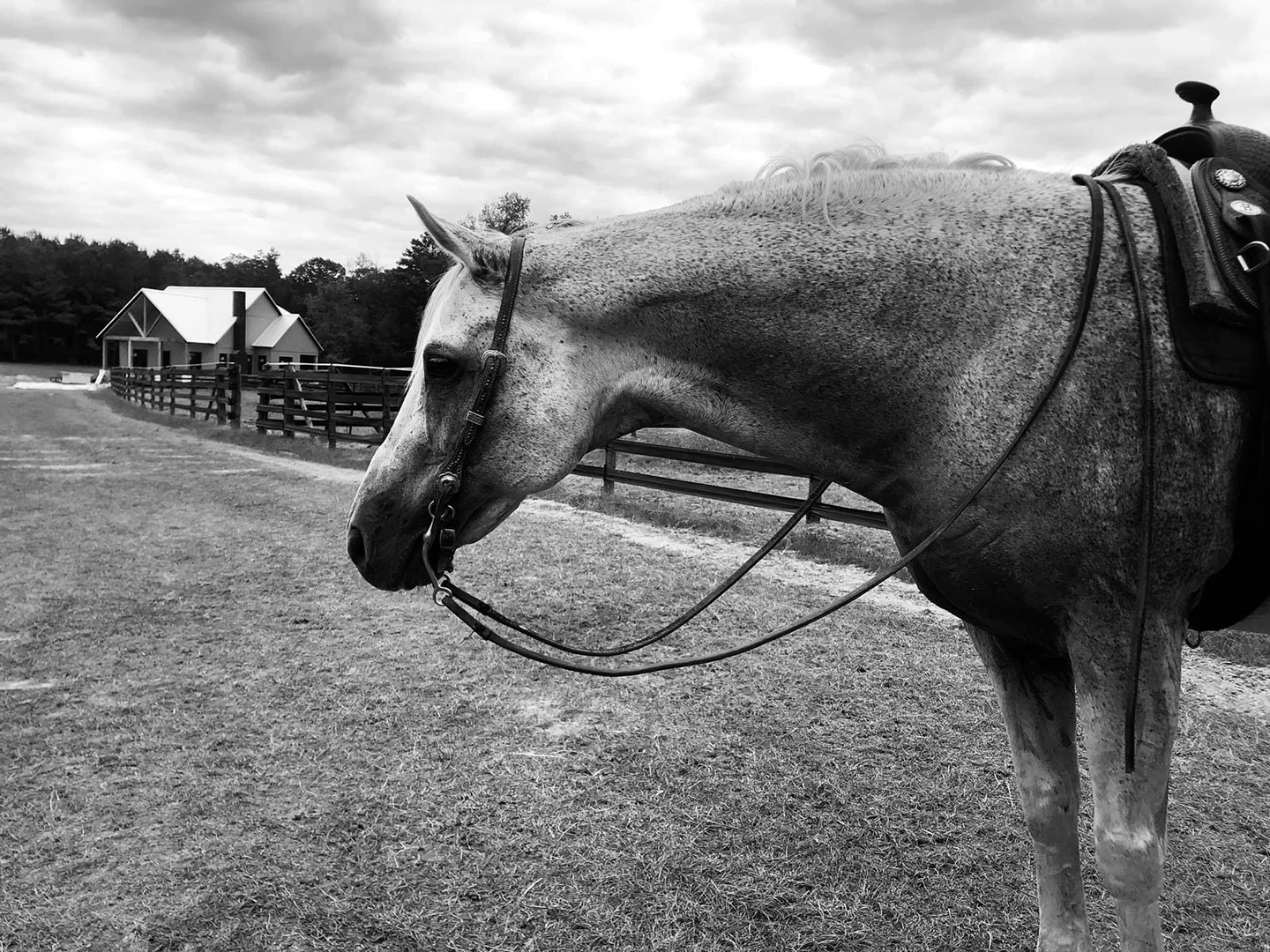
Good Karma: Aggie Veterinarians Save Horse From Life-Threatening Melanoma
Teresa Porter has been taking care of horses for decades, but none have touched her heart like Karma. Karma, known at competitions as So Riveting, is a 20-year-old quarter horse stallion with a striking gray coat. But with that color comes a problem — gray horses are genetically predisposed to developing melanoma, especially on body […]
Texas A&M Veterinarians Help Beloved Campus Police K-9 BTHO Mammary Cancer
When one of Texas A&M University’s police K-9s was diagnosed with cancer, veterinarians at the Texas A&M Veterinary Medical Teaching Hospital (VMTH) had the opportunity to serve an animal just as hardworking as they are. Jackie is a 9-year-old Belgian Malinois who worked alongside the Texas A&M Police Department as an explosives detection K-9 until […]