Introduction
Why It Matters
How We Find Out
What We Know
Story Time
Common Hazards: Hepatitis
Common Hazards: Heavy Metals
Activities
Self-Study Game
Introduction
 Toxic substances are everywhere. The body is not only exposed to toxic chemicals in the environment, but also some toxins are produced in the body through normal body chemical reactions.
Toxic substances are everywhere. The body is not only exposed to toxic chemicals in the environment, but also some toxins are produced in the body through normal body chemical reactions. How can our bodies cope? This module explains some of the ways that animals and humans combat and eliminate toxic chemicals. The organ systems involved include the lungs, the skin, and the digestive tract, but two organs are especially important: the liver and the kidneys.
We call the process of eliminating toxins, “detoxication” or “detoxification,” which is the opposite of “intoxication.” Different tissues detoxify in varying ways.
- Lungs can detoxify by removing gases (gas anesthetics are removed from the body by the lungs).
- Skin can detoxify by reducing the penetration of toxic substances (toxins in water don’t get in through the skin well; however, toxins in oils do penetrate easily).
- Digestive System can detoxify by eliminating toxic foods, by either vomiting or diarrhea.
- Kidneys detoxify by secreting toxins or filtering toxins out of the blood into urine.
- Liver detoxifies by changing the chemical nature of many toxins.
Kidney and liver are especially important. They are discussed separately because they work in different ways.Objectives
After completing this lesson, each student should be able to:- Explain why detoxication systems are needed in the body
- Identify the systems in the body that have detoxication functions and summarize how they perform their detoxifying actions
Why It Matters
But toxins would still be a problem even if we lived in a clean environment. Our own body makes toxic chemicals. For example, did you know that one product the body makes as a by-product of its normal chemical reactions is ethyl alcohol (the kind found in alcoholic drinks)? And the body changes alcohol into an even more toxic compound, acetaldehyde!
Have you heard all the advertisements for Vitamin E and C as substances needed to combat free radicals? Free radicals are normal chemical breakdown products and they are very toxic. Sometimes, these radicals cause cancer and contribute to aging.
See these sites for more information:
How We Find Out
Kidney Function
We learned earlier that kidneys detoxify by secreting toxins or filtering toxins out of the blood into urine. But how do we know this?The best way to learn what kidneys do is to examine the product of their function- urine. Examining the urine is also a good way to know if anything is wrong with kidney function. Medical technicians in hospitals and clinics routinely examine urine (“urinalysis”) looking for any abnormalities. Any abnormalities could signal kidney disease. Examples of diseases that can be detected by urinalysis include diabetes, kidney stones, and chronic infections of the urinary tract.
Kidneys stones, after they have been concentrated and removed from urine. Such stones in the urine can block urine formation and cause severe pain.
Urinalysis
 Urine is analyzed in three ways:
Urine is analyzed in three ways:
- Unmagnified (“macroscopic”): check for amount, color, clarity
- Chemical analysis with a “dip stick”: check for acidity, density, amount of protein, glucose, ketones, nitrites, and white blood cells. Special tests can be done for other substances, such as illegal drugs.
- Magnified (microscopic): check for crystals, squamous (flat) cells, bacteria, and other large objects.
Macroscopic Abnormalities:
- Not enough urine might mean that the kidneys are not filtering blood well.
- Too much urine might mean that the kidneys are not reabsorbing the water that is filtered out of blood – a common sign of diabetes mellitus.
- Urine should be yellow. If it is pale or clear it may mean dilution, either because too much water is being lost or it could be that you just drank a lot of liquid.
Chemical Abnormalities:
- Urine should be near neutral (pH=7), neither acidic nor basic.
- Presence of the substances listed above may indicate that the kidney is not cleaning the blood adequately or that the body contains more of the substance than even normal kidneys can handle.
Microscopic Abnormalities:
- Red blood cells should not be in urine, unless the urine is collected from females during menstruation.
- White blood cells should not be in urine. They could indicate infection of the kidneys, bladder, or other parts of the urinary tract.
- Too many crystals and stones could indicate a risk for blockage of the urinary tract. This prevents urine from being discharged, puts pressure on the kidney tubules, and stops urine formation.
Kidney Failure
Kidneys can become physically damaged by precipitates such as stones or by excess pressure (high blood pressure, obstructions in the bladder or the tube (urethra) that leads outside the body). The damage can progress to renal insufficiency and end-stage kidney disease, which require renal dialysis or a kidney transplant.Liver Function
Observing the liver tells us a lot about its function: - huge veins come into the liver from the gut
- venous blood flows past single rows of liver cells
- blood takes about 8 seconds to pass by the liver cells
- the flow path exposes blood to many phagocytotic, cells Comparing the chemical contents of the blood coming in with that of the blood leaving the liver shows that the liver must:
- make urea, a protein waste product
- make bile, which is released from the gall bladder to the intestines (makes fat easier to digest)
- remove low density lipids (LDL) and add high density lipids (HDL) to blood, thus protecting against hardening of the arteries
- convert and detoxify many drugs and toxins
Medical Application – Liver Function Tests
Because the liver is so vital for life, it is important to know if the liver is working normally. This is especially true in older age, when the liver is most likely to be damaged. There are several laboratory tests that doctors can have performed to check if liver function is normal.
Certain laboratory tests are used to determine whether the function of your liver is normal. Any symptoms of illness that might occur because of a poorly functioning liver will prompt a physician to consider ordering a medical laboratory to perform certain liver function tests on a blood sample. Such symptoms could include a yellowing of skin and membranes of the eye (called jaundice), a prolonged bleeding after cuts and bruises, and swollen or hardness of the liver (which the doctor determines by pressing on your abdomen over the liver). Unfortunately, you can have severe liver damage long before obvious symptoms appear. Sometimes, even the laboratory tests fail to detect severe liver damage.
The lab tests look for:- Certain enzymes – these leak from damaged liver cells into the blood
- Bilirubin (a normal by-product of red blood cell turnover) – builds up when liver is too damaged to remove it. This appears as jaundice.
- Albumin (this protein is made in the liver) – decreases in liver damage
- Blood clotting proteins (these are made in the liver) – clotting time is prolonged when liver is damaged
Many prescription drugs can damage the liver in the process of being deactivated by liver cells. But the most common causes of liver damage are alcohol abuse and certain virus infections (viral hepatitis).
What We Know
Many products of bodily metabolism are waste products that the body either does not need or cannot use. The body may even be damaged by some of metabolism’s products. Thus, mechanisms exist to rid the body of these damaging chemicals. In addition, many chemicals in our environment are damaging to the body and such products need to be eliminated or destroyed.
Three organ systems act in indirect ways to detoxify.
There are two very vital organ systems that have a direct role in detoxication. In fact, detoxication is the main reason we have these systems.
Liver: Cell Operations of the Liver
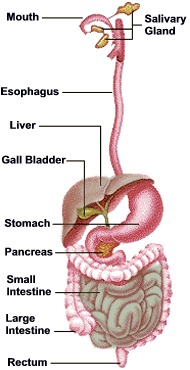 All substances that are absorbed in the digestive tract enter the veins that drain the gut and are carried in this venous blood to the liver. Think of the liver as the gatekeeper between the intestines and the general blood circulation. This is one of the few cases where venous blood comes INTO an organ. Because you have been told that the liver detoxifies chemicals, do you see why the liver gets its input of blood from the blood that drains from the gut?
All substances that are absorbed in the digestive tract enter the veins that drain the gut and are carried in this venous blood to the liver. Think of the liver as the gatekeeper between the intestines and the general blood circulation. This is one of the few cases where venous blood comes INTO an organ. Because you have been told that the liver detoxifies chemicals, do you see why the liver gets its input of blood from the blood that drains from the gut?
Relation of the liver to other organs in the abdomen. The liver lies just under the diaphragm and on top of the stomach. It is attached by a large vein to the stomach and small intestines.
The liver detoxifies numerous toxins. It also destroys drugs, such as alcohol, nicotine, and prescription medicines, because these things are not normal to the body. Some medicines have the bad side effect of damaging liver cells. It is like a war between liver cells and the medicine, because the liver is programmed to destroy foreign chemicals and cannot know that medicines are supposed to be good for the body nor know which medicines may damage the liver cells in the process of destroying the drug.
KIDNEY : Cell operations of the kidney
The first place that blood from the stomach and intestines goes is to the liver. But then the blood leaving the liver goes to the heart and is pumped directly to the kidneys. Kidneys regulate the balance of water and salts in the body, but they also have a very important role in detoxication.
With about 200 quarts being pumped through the kidneys every day, they do a big job for such a small organ! The main job is to take all of the blood in the body and clean it. This means: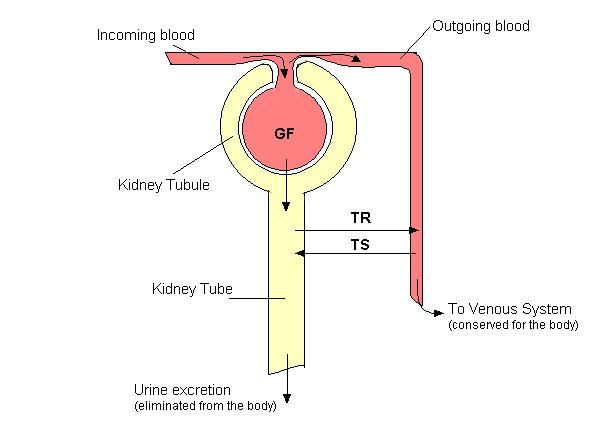
How do you suppose any organ could specialize to detoxify? One approach is taken by the kidney. The liver takes a different approach, involving two steps. If we examine the liver under a microscope, we see rows of liver cells with small spaces in between that act as a filter to remove dead cells, microorganisms, and chemicals as the blood flows slowly through the liver. This filter includes cells that engulf (“eat”) the sludge that is left trapped in the filter.
Once inside the Kuppfer cells, the sludge must be broken down. There are two phases of detoxification in the liver. Phase one includes an enzyme, cytochrome p-450, to detoxify the bad stuff. This means that the harmful chemical gets broken down into smaller parts that are not harmful to the body. Phase two detoxification is when the Kuppfer cells add materials to the chemical to be broken down, and this new chemical is not harmful to the body. This addition of materials to a harmful substance is called conjugation. Once phases one and two have been performed, the sludge is ready to be added back to the regular blood stream and secreted as waste, and it never harms the body. We have a wonderful, life-saving detoxification plant.
What happens in the kidney?
Each kidney contains about one million microscopic units, called GLOMERULI, which work together to clean the blood.
GF = glomerulus filtering. TR = tubular reabsorption. TS = tubular secretion.
So, you see that blood is filtered, giving up much of the water and dissolved substances it contains. Then, much of the water and some of the dissolved substances are reabsorbed into blood. Finally, some dissolved substances in blood are actually secreted into the urine.
See Animations of Kidney Function
 <
<
Summary of Chemical Changes of Filtered Blood
Blood Flow to Kidney
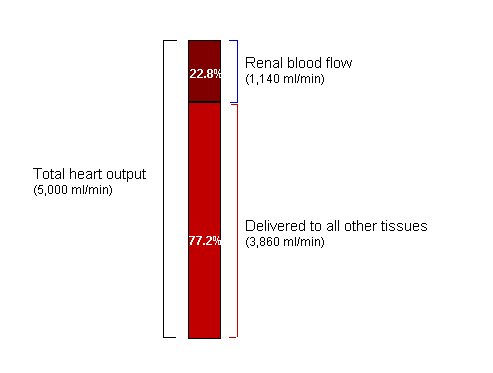
To be effective in cleaning blood, the kidneys must have a rich flow of blood. About 23% of the blood pumped by the heart over the course of a minute goes to the kidneys. So, within a few minutes, all of the blood in the body gets swept through the filtering system of the kidney.
Example Effects of the Kidney Function
| Substance | Average percentage of filtered substance re-absorbed | Average percentage of filtered substance excreted |
|---|---|---|
| Water | 99 | 1 |
| Sodium | 99.5 | 0.5 |
| Glucose | 100 | 0 |
| Urea (waste product) | 50 | 50 |
| Phenol (waste product) | 0 | 100 |
Drugs and the Kidney
Toxic compounds, drugs, or their breakdown products, are cleared from the blood by the kidneys. Can you think of some practical results of this? Do you see why the kidneys can help protect us from toxic chemicals? Do you see why drugs act for only a certain length of time? How long it takes to clear the blood of toxins or drugs varies with the chemical, but most substances are cleared within a matter of hours. Many medications have to be taken every few hours in order to maintain a fairly constant level in the blood because the kidneys are constantly eliminating the drug. You have heard about testing the urine of drug users or athletes. The drugs people take will show up in the urine.
What If the Kidneys Go Bad?
Obviously, loss of kidney function will lead to death. Inability to reabsorb water would lead to severe dehydration. Inability to secrete potassium can actually cause death because build up of potassium would stop the heart. Fortunately, two kidneys provide excess capacity. Only one kidney is actually essential. However, the loss of both kidneys is fatal. The only cure if both kidneys failed would be to get a transplant or to have the blood cleaned by machine (a process called kidney dialysis).
Story Time
Claude Bernard, 1813-1878
 Experimenting on animals is a controversial practice. Many people think that animals have rights and should not be subjected to experimentation. Medical researchers, however, hold the view that animal research is necessary to human welfare and is certainly more defensible than eating animals. Experimenting on animals, also known as vivisection, was established as acceptable scientific practice by Claude Bernard. It was he who showed how much could be learned and applied to medical practice through vivisection.
Experimenting on animals is a controversial practice. Many people think that animals have rights and should not be subjected to experimentation. Medical researchers, however, hold the view that animal research is necessary to human welfare and is certainly more defensible than eating animals. Experimenting on animals, also known as vivisection, was established as acceptable scientific practice by Claude Bernard. It was he who showed how much could be learned and applied to medical practice through vivisection.
In defending biomedical research on animals, the American Medical Association says:
“In fact, virtually every advance in medical science in the 20th century, from antibiotics and vaccines to antidepressant drugs and organ transplants, has been achieved either directly or indirectly through the use of animals in laboratory experiments.”

Claude Bernard was born near Villefranche (20km north of Lyons-see photo on right of his birthplace, now a museum), where his father worked the Chevalier de Quincieux estate. His father was a winemaker and Claude helped him tend the vineyards and process the harvest. His mother, Jeanne Saulnier, had a peasant background. His father went broke in a wine-marketing venture, and the family was poor. Claude studied Latin with a local priest and was taken in as a student in a Jesuit school at Villefranche. That school taught no science, and it is amazing that Claude developed an early interest in science. He studied at the middle school in Thoissey, but he quit school, without a diploma, and apprenticed to a chemist named Millet in a Lyon suburb. His work there was apparently boring, but he did enjoy the errands he ran to the nearby veterinary school.
While at Lyon, Claude developed an interest in medicine, perhaps in part because of his exposure to the veterinary school. Claude left Lyon to study medicine in Paris between 1834 and 1843. Claude was not a particularly good student, but then he had a very poor school background. Of 29 students passing the examination for the internship, Bernard ranked 26th. He failed the examination that would have qualified him to teach in the medical school, so he began collaborating with others in research projects.
Claude Bernard worked with François Magendie the leading physiologist of his time. For a while, Claude worked in Magendie’s shadow, but it soon became clear that Claude could hold his own with the best, even Magendie. In 1854 a chair of general physiology was created for Claude in the Sorbonne, and he was elected to the Academy of Sciences. When Magendie died in 1855, Bernard succeeded him as full professor before succeeding him to the experimental medicine chair at the Ollège de France in 1855.
Claude did not have his own laboratory at first, but his fame was such that he had a personal interview with Emperor Napoleon who made sure that a lab was constructed for him.
During most of the 1800s, France was the world leader in medicine, and Claude Bernard grew up in that culture where advances in medicine were being driven by the scientific method. Claude became a leader in using the scientific method and, in fact, is generally considered the founder of modern experimental physiology. One of the lasting contributions he made was his demonstration of the value of hypothesis-driven research. Claude’s experiments began with a hypothesis, and tests were designed that would either support or refute the hypothesis, and that in turn guided the next steps in experimentation. Claude had three guiding principles for his own research; he believed that 1) the notion of “vital force” does not explain life; (2) animal research (vivisection) is indispensable for physiological research; and (3) life is mechanistically determined by physic-chemical forces.
Of the many lasting discoveries made by Claude, one stands out because it is such a fundamental principle. The principle (called a scientific law in Physics) is that the internal workings of warm-blooded animals are more or less constant, and that physiological mechanisms resist external forces that would alter this state. This is the principle of homeostasis, which was further advanced by his successor Walter Cannon.
Among his many other discoveries were experimental demonstrations of many of the functions of the liver. He showed that secretions of the pancreas contained digestive enzymes. He showed that certain parts of the pancreas were involved in diabetes. He also showed that the contraction and relaxation of small blood vessels were regulated by nerves. In addition, he demonstrated that there was a functional junction between nerves and muscle and that curare blocks this junction. If they had been awarding Nobel Prizes in those days, Claude would have won several. His contemporary, Louis Pasteur, called him “physiology itself.”
Ironically, the organ systems that Claude spent so many years studying were the very ones that caused his own illness and death. Claude apparently developed chronic enteritis, with disease affecting the pancreas and the liver.
Biography of Claude Bernard, 1813-1878
| 1810-1820 | 1820-1830 | 1830-1840 | 1840-1850 | 1850-1860 | 1860-1870 | 1870-1880 |
|---|---|---|---|---|---|---|
| 1813 Born on 12th July at St Julien, Rhône, France | 1827 Pupil at the college in Villefranche | 1831 Leaves the college in Thoissey 1832 Apprentice in Millet’s Pharmacy in Vaise, then a suburb of Lyon 1833 Leaves St Julien for Paris 1834 Obtains his baccalaureate 1837 Appointed extern of the Paris hospitals 1939 Appointed intern of the Paris hospitals | 1843 Doctor of Medicine. Thesis on gastric juices. Discovers the glycogenic function of the liver. 1844 Fails the aggregation exam 1845 Marries Françoise Marie (Fanny) Martin 1846 Birth of a son Louis-Henri (dies at three months) 1847 Birth of a daughter, Jeanne-Henriette (Tony), died in 1923. Appointed substitute professor for Magendie at the Collège de France. Death of his father, Pierre Bernard. 1849 Naissance de Marie (meurt en 1922). Chevalier de la Légion d’honneur. | 1853 Doctor of Natural Science 1854 Elected member of the French Academy of Sciences. Occupies the chair of General Physiology in the Paris Faculty of Science (Sorbonne) 1855 Appointed professor of medicine at the Collège de France 1856 Birth of Claude-Henri (died in 1857) | 1861 Elected Member of the French Academy of Medicine 1865-1867 Convalescence after an illness (a sort of enteritis). Publication of his Introduction to the study of experimental medicine 1867 Death of his mother, Jeanne Saunier Appointed Commander of the French Legion of Honour 1868 Elected to the French Academy to the chair left vacant by the death of Flourens. His chair of General Physiology transferred to the French Museum of Natural History 1869 Officially separated from his wife. First letter to Madame Raffalovitch. Appointed Senator of the French Empire | 1876 Chief administrator of the Paris Universal Exhibition 1877 Last lecture at the Collège de France 1878 Dies on 10th February at 40 rue des Ecoles, Paris. National funeral takes place on 16th February at the church of Saint-Sulpice, Paris. He is buried in the Père-Lachaise cemetery, Paris, France |
References:
Bayliss, L.E. Living Control Systems, English University Press, London, 1966
LaFollette, Hugh and Niall Shanks. “Animal Experimentation: The Legacy of Claude Bernard”.
http://www.etsu.edu/philos/faculty/hugh/bernard.htm
The Claude Bernard Museum. http://www.claude-bernard.co.uk/page20.htm
Common Hazards: Hepatitis
Hazards for the liver include certain infections and certain chemicals that are toxic to liver cells. Hazards for the kidney include certain heavy metals. We discuss them separately because the hazards have different mechanisms of action.
Hepatitis
Hepatitis is irritation (inflammation) of liver. (The word ending “itis” means inflammation.) However, many causes of hepatitis go beyond inflammation and end in death of liver cells and eventual replacement with scar tissue (called “cirrhosis” of the liver).
Causes of hepatitis range from alcohol to viruses. Hepatitis can even be caused by our own immune system. This occurs when a genetically defective immune system begins to attack liver cells after the immune system is activated, usually by a virus.
The breakdown of alcohol causes the release of many chemicals that are toxic to the liver. A build up of these chemicals will cause hepatitis. After a long history of alcohol abuse, people will develop cirrhosis of the liver.
Certain viral infections can also cause hepatitis. There are six different hepatitis viruses:
- hepatitis A – vaccine available. Spread by feces of infected person (contaminated food or water)
- hepatitis B – vaccine available. Spread by blood (transfusions, contaminated needles, etc.) and blood fluids (sex, shared toothbrushes) from infected person.
- hepatitis C – no vaccine available. Spread by blood and body fluids of infected person. The leading reason for liver transplants.
- hepatitis D – no vaccine available. Spread by blood and blood fluids from infected person. Only occurs in the presence of a hepatitis B infection.
- hepatitis E – no vaccine available. Spread by feces of infected person.
Knowing how these viruses are spread should help you know what you need to do to prevent infection.
For more information see the Communicable Disease Center Web site.
Common Hazards: Heavy Metals
Heavy Metals
Four heavy metals (cadmium, mercury, lead and chromium) are all toxic to the kidneys. Each causes problems in the tubules, but by slightly different means.
Lead
- inhibits the functions of the mitochondria, making cells unable to reabsorb substances like they are supposed to
- also a major problem in damage to the brain, especially in young children
Sources: paints, gasoline (except unleaded), batteries, pipes soldered with lead, industrial plants
More about Lead
Mercury
- kidneys concentrate mercury
- reacts with other proteins and enzymes in the kidney cells and can eventually kill them
- can also damage the central nervous system.
- accumulates in food chains.
Sources: coal burning, manufacturing processes
More about Mercury
Cadmium
- damages kidney tubules (also causes anemia and bone and mineral loss)
- reacts with proteins and accumulates in kidney
- substitutes for zinc in enzymes and changes enzyme action
Sources: Some soils just naturally have high levels of cadmium; quarries, mines; plastics, batteries, rubber goods
More about Cadmium
Chromium
- reabsorbed by the tubule cells and becomes very concentrated
- interferes with energy exchange and can become a corrosive acid
Sources: metal finishing processes, burning of fossil fuels, wood preservatives
More about Chromium