April is recognized as National Heartworm Awareness Month as a reminder to protect our furry friends against heartworm disease before mosquito season peaks during the summer.
To understand the importance of preventing heartworm disease, pet owners should first understand how heartworms grow and are detected.
Heartworms are spread by mosquitoes that have bitten a heartworm-infected animal and picked up microfilariae, which develop into infective larvae in the third stage of its life cycle. The mosquito can then bite other animals and deposit the third-stage larvae, quietly infecting unsuspecting animals with heartworms.
After a pet is infected, the heartworms spend six to seven months developing into mature adult worms at which point they produce detectable levels of antigen – a protein that is primarily from adult female worms – and microfilaria – or baby worms. Testing positive for heartworms is dependent on whether antigen or microfilaria are present.
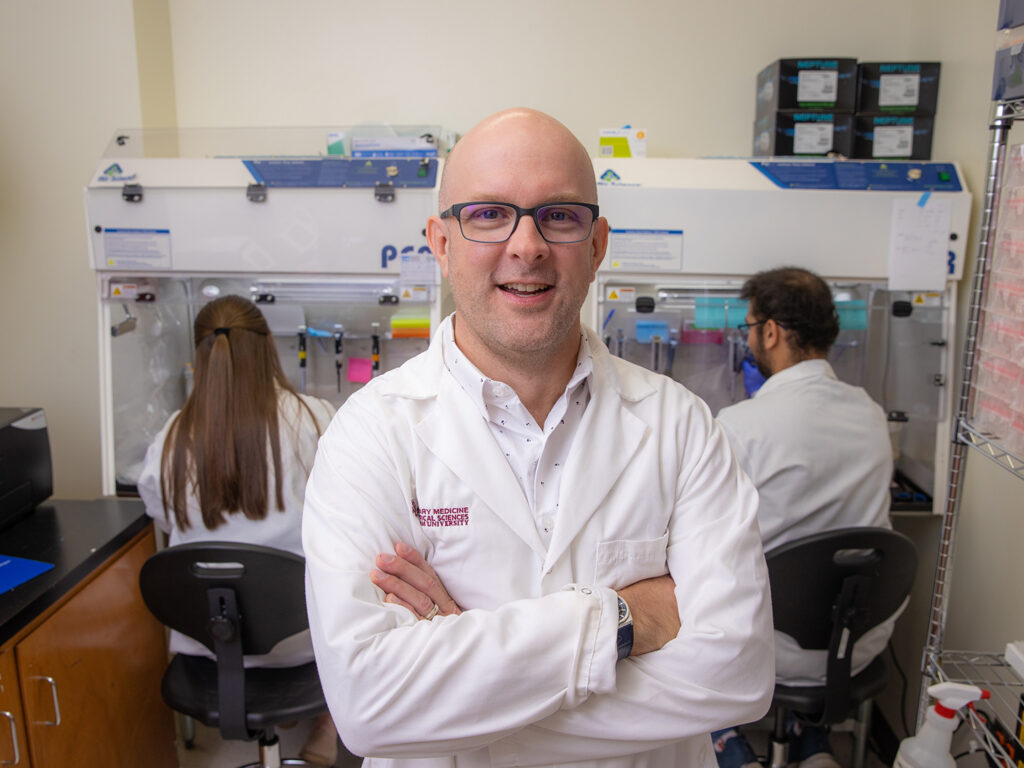
Since heartworms cannot be detected until months after infection, Dr. Meriam Saleh, a clinical assistant professor in veterinary pathobiology at the Texas A&M School of Veterinary Medicine & Biomedical Sciences, emphasizes that pets should have no gaps in their heartworm prevention plan to avoid infection entirely.
“Even if a puppy was infected when they were one day old, veterinarians are not going to be able to detect antigen or microfilaria until the worms are at least 6 months old and have developed enough,” Saleh explained. “If veterinarians don’t know if a pet is infected until six or seven months after infection, they can’t design an intervention or treatment program beforehand. It is better to just prevent the disease.”
Prevention starts by ensuring your pet is on a preventative plan for heartworms.
“The best preventative measure is to make sure pets are on a monthly or year-round heartworm prevention,” Saleh said. “If you are still concerned about a pet being bitten by a mosquito, owners can also use insect repellent made for pets or window screens, if they have windows open, to prevent mosquitoes from getting into the house.”
Nevertheless, Saleh stresses that repellent and window screens are ways to add a layer of protection and should not replace heartworm preventive medications.
If a pet is not on heartworm preventives, owners should look out for signs of heartworms – such as coughing, lack of appetite, and weight loss – and, most importantly, have their veterinarian test their pet for heartworms as soon as possible.
“Heartworms have the ability to live in an animal and ideally cause only a little bit of harm so that they can reproduce,” Saleh said. “But if left untreated, heartworms will accumulate and cause multisystemic heartworm disease – meaning multiple organs, such as the heart, lungs, liver, and kidneys, are affected – eventually leading to a pet’s death.”
Saleh explained that testing a pet for heartworms is also required before a pet can go on heartworm preventives.
If a dog tests positive for heartworms, then they can be treated with a set of injections given by a veterinarian called adulticide; however, it is a long journey before a dog fully recovers.
“You don’t want to undergo adulticide heartworm treatment lightly because it is really hard on the animal and is expensive,” Saleh said. “Managing an infected animal until they’ve recovered is a long process because they also need to be monitored on cage rest and have an exercise restriction.”
On the other hand, there is no approved medicine for cats who have tested positive for heartworms, so prevention is especially necessary to protect cats.
“Cats typically don’t have adult heartworms producing microfilaria and while tests could detect microfilaria, cats often succumb to the disease beforehand,” Saleh said.
Because heartworm disease can be devastating, owners should keep their pets on preventative medicine so that there is no risk of heartworm disease if bitten by an infected mosquito. Doing so will put you at ease knowing that your furry friend is both protected and healthy.
Pet Talk is a service of the College of Veterinary Medicine & Biomedical Sciences, Texas A&M University. Stories can be viewed on the web at vetmed.tamu.edu/news/pet-talk. Suggestions for future topics may be directed to vmbs-editor@tamu.edu.